Childhood stunting in developing countries
21/11/24, 12:16
Last updated:
09/03/24, 17:53
Published:
The tireless challenge
Introduction
Certain countries worldwide face numerous challenges that decrease their populations' quality of life; some include hunger, poverty and rising harmful emissions, which are complicated to resolve. This is because international cooperation is needed to tackle them effectively.
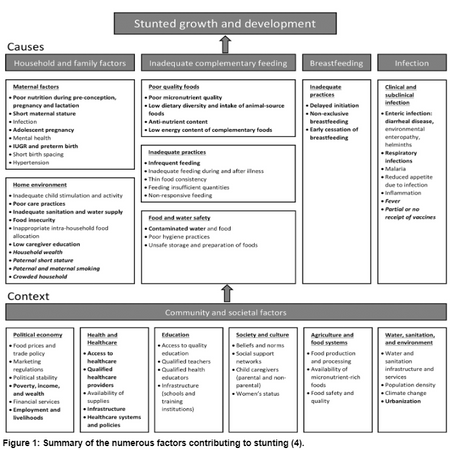
Furthermore, they are associated with stunting, defined as diminished growth and development that children experience because of undernutrition or lack of sufficient nutrients, frequent infections and deficient psychosocial interventions, according to the World Health Organisation.
With this definition in mind, this article will delve into stunting and malnutrition before discussing how stunting is linked to infectious diseases and harmful emissions and steps forward to reduce this condition in developing countries, as shown in Figure 2.
Undernutrition and stunting
Stunting is one of the consequences of undernutrition, possibly due to reduced synthesis of insulin-like growth factor 1 (IGF-1) in the body, leading to amplified growth hormone (6). As for the determinants of undernutrition, a paper from Brazil found socioeconomic characteristics like family income and biological ones such as age notably linked to undernutrition.
Another result of undernutrition is being underweight. A systematic review from Ethiopia focusing on nutrition in 5-year-old children amalgamated 18 studies. It estimated that stunting and being underweight had 42% and 33% prevalence, respectively; it could be inferred that undernutrition is linked to stunting.
Additionally, a paper that used data from 32 Sub-Saharan African countries discovered that providing maternal health insurance (MHI) reduces stunting and being underweight, which is more apparent in girls than boys. In turn, MHI is necessary for supporting children’s health.
Non-nutritional factors and stunting
As for infections and stunting, an article highlighted that children with stunted growth are vulnerable to diarrhoeal and respiratory diseases besides malaria. Moreover, conditions worsen undernutrition, causing a vicious cycle between them, manifesting into growth defects.
Furthermore, a systematic review of 80 studies found a connection between helminth infections and stunting, but insufficient evidence supported this hypothesis. With this said, there may need to be additional studies to investigate this further.
With undernutrition’s impact on the immune system, newborns and small children with extreme protein deficiency have smaller thymuses and underdeveloped peripheral lymphoid organs, leading to immunological cell defects such as reduced T-cell count.
Before concluding this article, exposure to harmful emissions is a recurring problem that affects everyone, including children. Different observational studies proposed that inhaling nitrogen oxide and particulate matter in utero could modify DNA methylation, possibly influencing foetal growth.
Conclusion
Reflecting on all the evidence in this article, stunting in developing countries is heading in a direction where it could become problematic. However, according to findings from UNICEF, stunting has gradually reduced between 2000 and 2020 in children under 5 years old. Nevertheless, awareness of stunting in developing countries is critical because it is the first step to tackling this health issue.
Written by Sam Jarada
Related articles: Childhood obesity / Depression in children
REFERENCES
Jamali D, Leigh J, Samara G, Barkemeyer R. Grand challenges in developing countries: Context, relationships, and logics. Business Ethics, the Environment & Responsibility. 2021 Sep;30(S1):1–4.
Maleta K. Undernutrition. Malawi medical journal: the journal of Medical Association of Malawi. 2006 Dec;18(4):189–205.
World Health Organization. Stunting in a nutshell. www.who.int. 2015 Nov;19.
Beal T, Tumilowicz A, Sutrisna A, Izwardy D, Neufeld LM. A review of child stunting determinants in Indonesia. Maternal & Child Nutrition. 2018 May 17;14(4):e12617.
Vaivada T, Akseer N, Akseer S, Somaskandan A, Stefopulos M, Bhutta ZA. Stunting in childhood: an overview of global burden, trends, determinants, and drivers of decline. The American Journal of Clinical Nutrition. 2020 Aug 29;112.
Soliman A, De Sanctis V, Alaaraj N, Ahmed S, Alyafei F, Hamed N, et al. Early and Long-term Consequences of Nutritional Stunting: From Childhood to Adulthood. Acta Bio Medica : Atenei Parmensis. 2021;92(1)
Correia LL, Silva AC e, Campos JS, Andrade FM de O, Machado MMT, Lindsay AC, et al. Prevalence and determinants of child undernutrition and stunting in semiarid region of Brazil. Revista de Saúde Pública. 2014 Feb 1;48:19–28.
Abdulahi A, Shab-Bidar S, Rezaei S, Djafarian K. Nutritional status of under five children in Ethiopia: a systematic review and meta-analysis. Ethiopian Journal of Health Sciences. 2017 Mar 15;27(2):175.
Kofinti RE, Koomson I, Paintsil JA, Ameyaw EK. Reducing children’s malnutrition by increasing mothers’ health insurance coverage: A focus on stunting and underweight across 32 sub-Saharan African countries. Economic Modelling. 2022 Dec 1;117:106049.
Vonaesch P, Tondeur L, Breurec S, Bata P, Nguyen LBL, Frank T, et al. Factors associated with stunting in healthy children aged 5 years and less living in Bangui (RCA). Wieringa F, editor. PLOS ONE. 2017 Aug 10;12(8):e0182363.
Raj E, Calvo-Urbano B, Heffernan C, Halder J, Webster JP. Systematic review to evaluate a potential association between helminth infection and physical stunting in children. Parasites & Vectors. 2022 Apr 20;15(1).
Schaible UE, Kaufmann SHE. Malnutrition and Infection: Complex Mechanisms and Global Impacts. PLoS Medicine. 2007 May 1;4(5):e115.
Sinharoy SS, Clasen T, Martorell R. Air pollution and stunting: a missing link? The Lancet Global Health. 2020 Apr;8(4):e472–5.
UNICEF. Malnutrition in Children. UNICEF DATA. 2023.
Project Gallery